
This free dissertation on “Implant Dentistry” will show you exactly how our examples will look upon completion.
Introduction
Background
Aims
Objectives
Review of the Literature
Methods
Results and Outcomes
Discussion
Conclusions and Recommendations
Reflection
References
Appendices
The aim of this study was to examine the current technology in comparing one-piece versus two-piece implant systems and to evaluate the relevant literature and different studies after applying selection criteria. To achieve this aim, an examination of the long-term success of the different implant systems and examined literary evidence in assessment of the cervical bone loss around the two different implant types after implant placement. A summary of the research, conclusions and recommendations are also provided.
A Comparison of One-Piece versus Two-Piece Dental Implants
Modern dentistry involves the evaluation, diagnosis, prevention and treatment of diseases and conditions in the oral and maxillofacial region. This includes the restoration of function, comfort, aesthetics, speech and health. With seventy percent of persons in theU.S. population missing at least one tooth, one commonly encountered condition requiring treatment in today’s society is that of edentulism. The previous treatment of choice for any form of edentulism was some form of denture. For example, the most common treatment for one missing posterior tooth was a three unit fixed partial denture; however with the success, predictability and continued research of osseointegrated dental implants there has been a dramatic increase in the inclusion of dental implants as a viable treatment option. Osseointegrated dental implants initially received a poor reputation because the first attempt at anchorage within bone failed due to scar tissue forming between the bone and the implanted material. This allowed for epithelial down-growth potentially leading to native bacteria infecting these epithelial pockets resulting in an inflammatory reaction that could cause bone resorption and mobility of the implant.
The status of dental implants did not change much until the late 1950s when aSwedish professor, Per-Ingvar Branemark, unexpectedly found a way to predictably form intimate bone-to-implant apposition of significant strength that could withstand load transfers. The basic principle was that if a hole was prepared in bone without traumatizing the tissues or overheating the bone an intimate bone apposition could be achieved with a biocompatible implantable device; he named this process osseointegration. Since then, millions of patients have been treated with dental implants using this principle (Chun et al. 2008).
Following their introduction just over a half century ago, dental implants have since changed the lives of millions of people worldwide. Dental implants are surgically implanted into the jawbone and greatly improve appearance since they prevent the jawbone from shrinking. Moreover, dental implant patients are able to eat anything since dental implants look, feel and function like natural teeth (Dental Implant Offers Alternative to Dentures 2004). After trauma or years of bone resorption, though, patients can arrive for implant treatment with different level of bone volume, length and height of ridge, and inter-occlusal space. Some sites cannot accept the standard sizes of many available implants without site development. Bone augmentation is an option for increasing the available bone volume if a standard diameter implants is required by the clinician. For dental implants to be successful, the jawbone must have enough bone to support them. Tooth loss often leads to more loss of bone. The tooth loss may be caused by periodontal (gum) disease, dental caries (cavities) and infection, injury or trauma, or a developmental defect. If the bone under the gum is not tall enough, not wide enough or both, patients will need a procedure to add bone to their jaws before implants can be placed. The supportive quality of augmented graft, though, is debatable (Flanagan 2008) and therefore alternative size implants have been introduced. Over the past decade, endosseous implants of increasingly smaller diameters have been introduced into the field of dentistry. Endosseous implants are medical devices, regulated by FDA to ensure their safety and effectiveness. They are Class III devices, a category that covers life-supporting, life-sustaining, and implanted items (Modeland 1998).
Implant diameter is the dimension measured from the peak of the widest thread to the same point on the opposite side of the implant. The diameter measures the outside dimension of the thread. This type of implants can be divided to two different groups, narrow diameter implants and mini implants. Narrow diameter implants are generally 2.75 mm to 3.3 mm in diameter. They are frequently used in cases of limited alveolar anatomy like in the edentulous space smaller than 5-6 mm, which is minimum requirement for conventional implants (Huang et al. 2010; Preoteasa et al. 2010).
Typical areas for use of these implants are lower incisors. Mini dental implants are smaller than their small diameter counterparts, with diameters ranging from 1.8 mm to 2.4 mm and are provided for immediate stabilization of a dental prosthetic appliance after a minimally invasive procedure or for cases where traditional implants are impractical, , or when a different type of anchorage system is needed. Analysis of the success of this type of implant restoration has not been clearly determined. The term mini has also been used to describe very short length implants with standard or larger diameters.
The importance of implant dentistry transcends the strictly clinical outcomes and the procedures may have lifelong and life-changing implications. For instance, Cash (2002) emphasizes that, “It is widely recognized that facial attractiveness is a social asset that results in greater acceptance by others, including peers, teachers, and employers. Conversely, unattractive facial features can be a social liability and results in peer rejection, academic difficulties, and (later) employment problems” (p. 342). Implant dentistry is a restorative procedure with oro-surgical aspects. It is highly predictable and the implants in all modern systems encounter very few problems with integration. The key Questions for clinician choosing a system are how easily I can restore the implants? Is it better for patient cost wise, how this implant is clinically acceptable/good? In one-piece implants, the fixture and the abutment are made from one piece of titanium and integrated in one implant body that is inserted during a one stage implant surgical procedure. In 1950’s, Tramonte was the first to introduce the one-piece implant and it was used for immediate loading, however most clinicians have continued to utilize two-piece implant systems for one-stage procedures. The implant-abutment junction constitutes a structural weakness, while the need to remove a healing abutment and replace it with a final abutment adds complexity to the procedure and adversely affect the healed or healing gingiva. The one-piece implant utilized in the many cases avoids both drawbacks.
In sum, the aim of this study was to examine the current available implant systems in the market and to compare one piece versus two piece implant and evaluate literature and carry out a differences study after applying selection criteria. A secondary aim of the study was to assess the reduced surgical time and lab work and what factors affect the selection of one-piece or two-piece implant systems.
The objective of this study was to assess the reduced surgical time and lab work and what factors affect the selection of one piece or two piece implant systems. To this end, the study explored the long-term success of the different implant systems and examined literary evidence in assessment of the cervical bone loss around the two different implant types after implant placement.
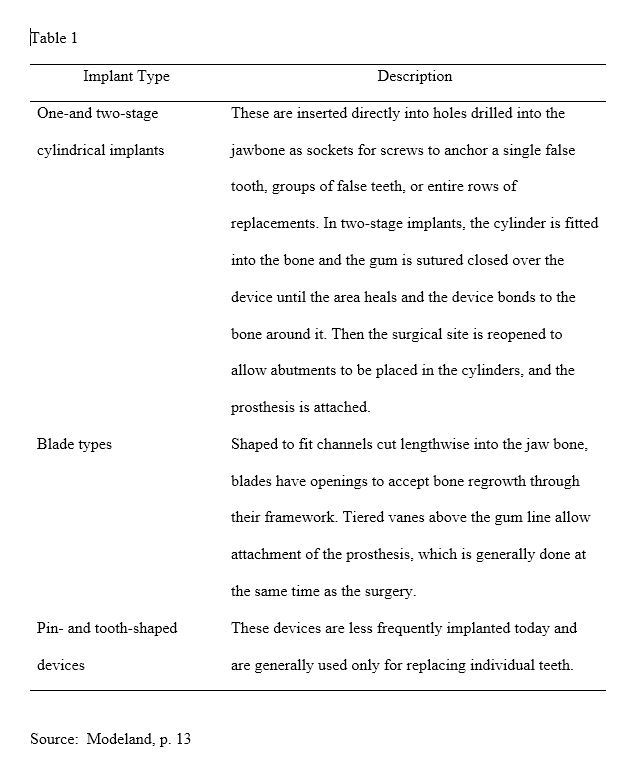
Four general designs of devices are currently in use in implant dentistry as shown in Table 1 below:
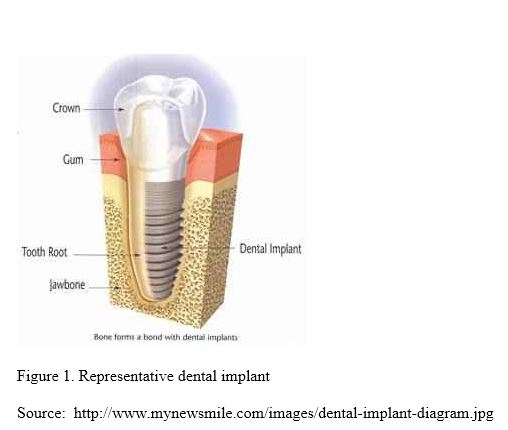
Dental implants are a reliable and long-lasting replacement for missing teeth. A dental implant consists of two parts. First there is a root form that is placed in the jaw. It is approximately the same size as a tooth root, and it takes the place of the root of the missing tooth. Usually a healing period is required for the process known as osseointegration—during which the bone grows in tightly around the root form so that it is solidly anchored. By tightly adapting the surgical site to the root form, this healing period can be shortened. Some practitioners offer what is called “teeth in an hour,” where the dental implant is placed into function immediately. This can be done, but there may be a trade-off between risk and patience here. When the healing time is rushed, there could be increased risk of failure. The visible part of the dental implant is the crown. An abutment is screwed into the root form and the crown is placed over it. If the process is done well, the end result is very functional, long-lasting, and highly esthetic (Dental Implants 2011).
Advantages and Disadvantages of Dental Implants
Disadvantages:
Advantages:
Osseointegrated dental implants have become reliable and safely provide long-term prosthetic stability for edentulous clients of all ages. Dental implants are not an appropriate treatment for all persons. The basic objective of dental implantation is to provide an attachment mechanism for teeth or dentures. Dental implants can anchor lower or upper dentures, provide a method to replace partial or full dentures with fixed bridgework, provide a method of replacing a single tooth, improve chewing function and restore the feeling of natural tooth function, and improve the quality of life by removing the frustration associated with using dentures or removable bridgework (Ubell 1992).
Today, implants are placed using both non-submerged and submerged approaches, and in one- and two-piece configurations. Previous work has demonstrated that peri-implant crestal bone reactions differ radiographically under such conditions and are dependent on a rough/smooth implant border in one-piece implants and on the location of the interface (micro gap) between the implant and abutment/restoration in two-piece configurations.
Peri-implant bone loss is a highly complex phenomenon with numerous etiologies currently debated in the dental literature (Zamani 2008). Endosseous, root-form dental implants distribute occlusal stresses into the supporting bone as a function of their overall design and the amount of bone to-implant interface achieved. Various reports in the dental literature suggest that both high and low stresses can lead to margin bone resorption. Preservation of peri-implant marginal bone height thus depends, in part, on proper distribution of marginal stress; however, major variations in the abilities of different implant designs to resist and distribute vertical and lateral occlusal loads have been documented using three dimensional (3D) finite element stress analyses (FEA) (Zamani 2008). The ability of one-piece dental implant designs to maintain peri-implant crestal bone levels to the same degree as two piece implant designs has recently been questioned. The aim of the study by Zamani (2008) was to compare how the level of stresses generated by one-piece and two-piece implant designs simulated homogenous bone and to determine if load distributions were significantly different.
Three-dimensional FEA code was used to simulate one-piece implants (1P) and two-piece implants with internal hexagon connections and assembled with friction-fit abutments (2P). The implant and abutment of the 2P model were designed with bonded interfacial surfaces to replicate the documented “virtual cold weld” between the assembled components, and this bonded relationship was also assumed in the analysis. All implant models were surrounded by a block of simulated homogenous bone that had linear elasticity with an average Young’s modulus value of 3 GPa, which is the mid-range stiffness value of cancellous bone.
For the study models, a uniform, 2-mm thick bone material surrounded each implant, and it was assumed that bone-to-implant contact (BIC) was 100% with bonded interfacial surfaces. All the simulated implant-and-bone-block models adhered to the manufacturer’s protocol for implant placement. Identical load and boundary conditions were used for all of the study implants. The material properties for titanium alloy (Ti-6Al-4V) were used for implants, restorative parts, and retaining screws. Figure 2 below shows typical boundary conditions and mesh configurations used in various simulations. A compressive load of 222.4 N (50 lbs) at an offset with respect to the implant axis and at a 30-degree angle was applied to all the various assemblies.
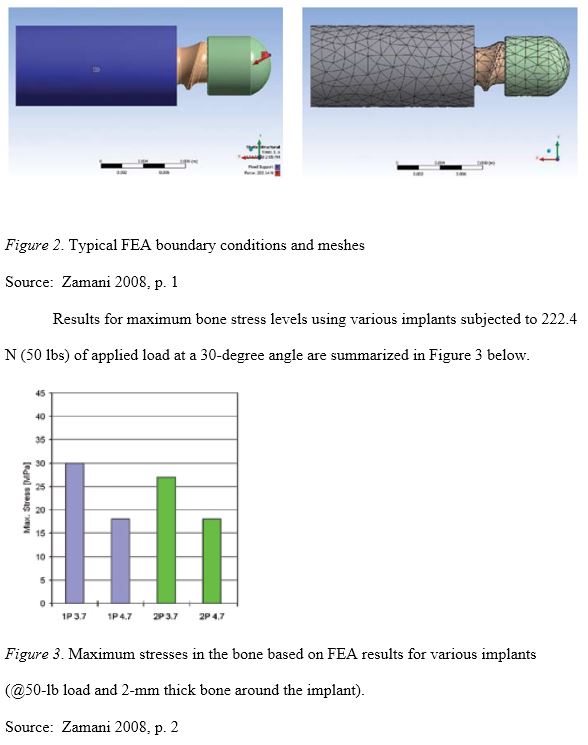
Average dental bone yield stress in compression is approximately 180 MPa. The vertical component of biting force in the incisor regions of adults is approximately 222 N (50 lb), which was used for this analysis with the assumption that 3.7 mm-diameter implants are often used in incisor region. Utilizing those parameters with a 2-mm thick bone, there was only a 3 MPa difference between 1P and 2P models that were 3.7 mm in diameter. Based on a comparison of these results with previous studies, Zamani (2008) concluded that no significant difference was found in bone stress concentrations between simulated 1P and 2P implants with the same length and diameter. It should also be noted that 2 mm of peri-implant bone is the borderline for the 3.7 mm-diameter study models; as the peri-implant bone increases in thickness, the maximum stress values of 1P and 2P merge exponentially according to the present calculations. For example, at 222.4 N (50 lb) of load, 1.6% is the maximum difference between these implants utilizing the present calculations (Zamani 2008).
During the course of the Zamani (2008) study, it was observed that a residual plate that is less than 2 mm in thickness could have an adverse affect on bone stress levels and crestal bone maintenance. It is important to note that this same phenomenon has also been clinically documented in a prospective, multi-center clinical study that was conducted by the U.S. government and involved the placement of approximately 3,000 implants. The present study also noted that both vertical and lateral load stresses decreased in inverse proportion to an increase in implant diameter (Zamani 2008). Within the limitations of this study, it was found that one-piece implants create similar stresses to two-piece implants in the same length and diameter. Reported differences in marginal bone levels between one-piece and two-piece implants may be attributable to variables independent of implant design since other reports in the dental literature have not observed this same phenomenon (Zamani 2008).
Most implant hardware in use today is made from titanium alloys. Coatings of calcium phosphates, carbon compounds, and titanium are sometimes added to promote successful bonding of the implant to bone. However, the coatings have not been shown to improve the bonding of the implant to bone, according to Sands. Due to the routine presence of bacteria in the mouth, there is a risk of infection of the tissue or bone surrounding the implant. There also is some risk that the additional stress of the implant on bones in the jaw will speed up bone resorption and lead to implant failure and possibly a toothless future. Persistent pain or discomfort, speech problems, nerve injury, and damage to adjacent teeth are rare but possible complications of implants (Modeland 1998).
Carbon nanotubes have also been proposed by Price et al. (2004) as a possible new orthopedic/ dental implant surface material because of their unique mechanical, electrical, and cytocompatibility properties. Cell viability and number of human osteoblast CRL-11372 were determined after 3, 6, 11, and 24 hr of incubation by ethidium homodimer and calcein AM staining. The authors used conventional fibers (diameter > 100 nm) and nanoscaled fibers (diameter < 100 nm). The fibers agglomerated within 1 week in cell culture media to ropes of about 340 nm in diameter in the case of conventional fibers and about 670 nm in the case of nanoscaled fibers. The nanoscaled carbon fibers appeared to influence osteoblast viability less than their conventional dimensioned counterparts. The suspended carbon fiber agglomerates were taken up by the osteoblasts and were incorporated in lysosomal vacuoles (Price et al. 2004). This future application of carbon nanotubes as implant material is in itself a promising issue, but one of the key questions is do carbon nanotubes influence the differentiation of osteoblast progenitor cells and to what degree is the formation and activation of osteoblasts affected? (Helland et al. 2007).
Conditions that can rule out dental implants include hypertension, heavy smoking, alcohol and drug abuse, chronic illnesses such as diabetes, bone deterioration, and bruxism (habitual tooth grinding), according to the University of Detroit’s Dr. Mentag. Endosseous implants are medical devices, regulated by FDA to ensure their safety and effectiveness. They are Class III devices, a category that covers life-supporting, life-sustaining, and implanted items. Under the 1976 Medical Device Amendments, FDA will require manufacturers of dental implants to submit data from controlled clinical studies to demonstrate the safety and effectiveness of their products or stop marketing them as early as 1990, according to FDA’s Singleton. In sum, dental implants have arrived. They may not be the solution for every case of tooth loss, but for those who are candidates, implants promise an alternative to dentures.
According to Cash and Pruzinsky, it is important to assess each dental implant candidate from a holistic perspective. “Assessing body image,” Cash and Pruzinsky advise, “first requires an understanding of what facets of the body are critical for the clinical issue of interest” (2002, p. 345). Three key measures are typically used in the dentofacial body image assessment as follows:
This study used a critical review of the relevant peer-reviewed and scholarly literature to achieve the above-stated aim and objectives. This method is highly congruent with numerous social researchers who emphasize the need to thoroughly review what is known about a given topic in the course of the research. For instance, according to Gratton and Jones (2003), a critical reviewing of the timely literature is an essential task in all research. “No matter how original you think the research question may be, it is almost certain that your work will be building on the work of others. It is here that the review of such existing work is important. A literature review is the background to the research, where it is important to demonstrate a clear understanding of the relevant theories and concepts, the results of past research into the area, the types of methodologies and research designs employed in such research, and areas where the literature is deficient” (p. 51). In this regard, Wood and Ellis (2003) identified the following as important outcomes of a well conducted literature review:
It justifies any new research through a coherent critique of what has gone before and demonstrates why new research is both timely and important. Likewise, Silverman (2005, p. 300) suggests that a literature review should aim to answer the following questions:
As noted in the introductory chapter, the aim of the study was to examine the current available implant systems in the market and to compare one piece versus two piece Implant and evaluate literature and carry out a differences study after applying selection criteria. In addition, the study assessed the reduced surgical time and lab work and what factors affect the selection of one piece or two piece implant systems. The results of the research showed that implant dentistry is a restorative procedure that involves a number of oro-surgical aspects, but the procedure was shown to be highly predictable and the implants of all modern system encounter very few problems with integration. The key questions for clinician choosing a system will therefore involve a cost-benefit analysis concerning patient preferences and clinical acceptability.
The research showed that at present, there are seven dental implant systems with a seal of approval by ADA on the market; these were Straumann implants, Nobel Biocare’s Branemark model and AstraTech implants being most popularly implemented and researched ADA approved implant systems (Dental implant systems 2011). A major problem for implants, though, is the lack of jaw bone that occurs in 10% of prospective patients. Research is underway to find bone stimulators. These include hormones and the use of Gore-Tex, which encourages bone growth by blocking other cells from filling empty spaces in bone (Ubell 1992). In addition, the candidate for implants can have no history of drug abuse (potential for misuse of pain management drugs) and must possess realistic expectations of the outcome (Ebersole 1998).
The clinician’s long-term implant survival success rate depends on the preservation of the hard and soft tissue around implant after placement. Successful endosseous implant therapy requires integration of the implant with bone, soft connective tissue and epithelium. To help promote successful outcomes, the research showed that the three most widely used implant systems are Branemark, Straumann and AstraTech, each of which possesses its own characteristic surface topography finish. A comparison of these implant systems is provided in Table __ below.
Comparison of Branemark, TiUnite, Straumann and AstraTech Implant Systems
| System | Description | One Piece | Two Piece |
| Branemark (http://www.nobelbiocare. com/en/products-solutions/implant-systems/default.aspx) | Brånemark System dental implants are the most scientifically documented in the world and are backed by more than 40 years of published results on their safety, predictability, clinical success, and longevity.
Key benefits: 1. Ideal for use in dense bone. 2. Enhanced osseointegration. 3. External hex connection. 4. Exceptional restorative versatility for all applications. The Branemark systems are indicated for both flapless and immediate function cases. Graftless procedures are also simplified with Zygoma and Shorty implants. The system offers complete solution packages for crown, bridge, and implant cases – from temporary to final restorations. Nobel Biocare offers a range of implants in two drilling protocols – parallel and tapered. Parallel is the most versatile drilling protocol, enabling fewer drilling steps in common indications and offering a passive fit in dense bone. Also, it can enhance stability in soft bone when under-preparation is possible. Tapered dental implants follow an easy-to-use, step-by-step drilling protocol. Surgical kits are logically and simply structured and drilling is the same for all indications.
|
NobelActive is an advanced, next-generation dental implant featuring a unique, innovative body design and prosthetic connection.
NobelActive is suitable for all indications and offers exceptional primary stability – even in compromised bone situations. It is particularly suited for use in the esthetic zone. Based on its ability to redirect during insertion, it provides clinicians with maximum placement flexibility. Key benefits: 1. NobelActive is an advanced dental implant that offers dental professionals various benefits. 2. NobelActive offers experienced surgical and restorative clinicians an enhanced set of options for cases involving soft to medium bone. 3. The prosthetic connection of NobelActive has been designed for maximum restorative flexibility. 4. The NobelActive surgical kits contain all the components needed to meet surgical requirements. |
NobelReplace Tapered – a part of the NobelReplace dental implant system – is the world’s most widely used, versatile, two-piece dental implant system.
Suited for both starting or experienced restorative clinicians and surgical implant users, NobelReplace provides a simple, flexible, color-coded, multi-use implant system. It performs well in soft and hard bone, one- or two-stage procedures, flapless and flapped surgeries, as well as immediate and delayed loading procedures. And it supports Nobel Biocare’s powerful NobelGuide digital 3D diagnostics, treatment planning and guided surgery system. Key benefits: 1. A versatile, easy-to-use, predictable implant. 2. Its prosthetic versatility and tri-channel connection make NobelReplace well suited for all indications. 3. NobelReplace offers flexibility in individualized and prefabricated restorative options. Furthermore, due to its tactile internal tri-channel connection and color-coded implant diameters, it is accurate and easy to use. 4. Nobel Biocare offers a variety of kits for the NobelReplace dental implant system. |
| Straumann
(http://www.straumann.us/us-index/ products.htm) |
The company states that with respect to reliability, its products feature:
1. Implants designed for optimal tissue response. 2. Reduced healing time. 3. Morse taper connection for maximum stability. The company also cites the simplicity of their use: 1. A logical component structure. 2. Procedures that are easy to learn. 3. One surgical kit. Finally, the company emphasizes the versatility of its implant products: 1. Successful outcomes with any indication. 2. Free choice of surgical procedure. 3. A wide range of prosthetic options. The Straumann Bone Level Implant provides a solution for all bone level treatments. Its design is based on the latest technology and scientific know-how in implant dentistry. Moreover, it respects key biological principles, guarantees predictable esthetic results and offers simple handling in all indications. Other notable attributes include: 1. Optimized crestal bone preservation with Bone Control Design. 2. Reliable treatment predictability. 3. Pleasing aesthetic results. 4. Simplified handling. 5. Roxolid and SLActive combine high strength with excellent osseointegration to deliver more peace of mind in treatment with small diameter implants. 6. Flexibility of having more treatment options. 7. Roxolid provides a wider choice of treatment options with small diameter implants. This can facilitate selection of the optimal treatment for patients in specific clinical situations. 8. Designed to increase patient’s acceptance to implant treatment 9. The benefits of small diameter implants are gained by Roxolid that provides greater confidence when placing small diameter implants in patients. |
According to Controversies over Implant Connections and Surfaces (http://www.implantdirect.com/controversy/contro1_pt08-2.html), prior to 1986, Straumann sold TPS-coated implants with a machined abutment top that was part of the implant (i.e. one-piece design.) In 1986, the company’s consulting International Team of Implantologists (“ITI”) developed the Bonefit™ System, which originally included threaded and non-threaded hollow-basket designs with a 2.8mm-high machined neck for one-stage surgery. A solid-screw, non-self-tapping design added later became known as the ITI implant. Because both of these implants require attachment of secondary prosthetic abutments, they are considered two-piece designs. | |
| AstraTech
(http://www.astra tech.us) |
Astra Tech develops, manufactures and markets dental implants and advanced medical devices within urology and surgery. Building on the proven success of TiOblast, OsseoSpeed is the first and only implant in the world with a chemically modified titanium surface, providing unique nano scale topography, that stimulates early bone healing and speeds up the bone healing process.
The result of the micro-roughened titanium surface treated with fluoride is increased bone formation and stronger bone-to-implant bonding. Together with MicroThread™ on the implant neck, OsseoSpeed provides true growing power in action for more reliable and effective treatment. The clinical benefits of OsseoSpeed are proven and well-documented. |
Complete descriptions of the company’s one-piece designs are available at http://www.astratechdental.us/Main.aspx/ Item/827544/navt/72677/navl/92618/nava/92619. The company reports that all of these dental implants have proven abilities to speed up the bone healing process. The unique OsseoSpeed implant surface, one of four key features in the Astra Tech BioManagement Complex, stimulates the early bone formation and provides stronger bone-to-implant bonding. The implant neck is designed with MicroThread that offers optimal load distribution and stress values. The Conical Seal Design of the Astra Tech Implant System allows for a strong and stable implant-abutment connection. In addition, the Astra Tech dental implants have proven clinically to maintain marginal bone levels (mean marginal bone reduction of only 0.3 mm over 5 years). | |
Taken together, the research and empirical observations indicate that one piece implants are preferable in many cases because surgeries are minimally invasive, patients tend to experience little or no discomfort and the use of the one piece implant system also significantly reduces treatment time based on the elimination of the post-surgical visits traditionally involved in the removal of the healing abutment and place permanent abutment.
Gingival aesthetics around natural teeth is based upon a constant vertical dimension of healthy periodontal soft tissues and the biologic width. Because of the subjective qualities involved in any aesthetical application, universal guidelines derived from the Golden Ratio can help guide the process (Cash & Pruzinsky 2002).
‘Bone augmentation and nerve repositioning.’ 2010 Simple Step Dental. [online] available: http://www.simplestepsdental.com/SS/ihtSSPrint/r.WSIHW000/ st.32575/t.34985/pr.3/c.358888.html/
Cash, T. F. & Pruzinsky, T. 2002 Body Image: A Handbook of Theory, Research, and Clinical Practice. New York: Guilford Press.
Chun, J., Schwartzberg, D., Shum, N., Swaida, F., Tse, J. & Wong, S. (2008). ‘Which of the currently available implant systems would you prescribe to your patient? An Evidence-based Report.’ University of Toronto. [online] available: http://www. utoronto.ca/dentistry/newsresources/evidence_based/EBReports08/W1_EBL_Rep ort.pdf.
‘Dental Implant Systems.’ 2011 Bangkok Dental Implant. [online] available: http:// www.bangkokdentalimplant.com/dental-implant-system.htm.
‘Dental Implants.’ 2011 Infinity Dental Web. [online] available: http://www.mynew smile.com/dental_implants/index.html.
Ebersole, P. 1998 Toward Healthy Aging: Human Needs and Nursing Response. St. Louis, MO: Mosby.
Flanagan, D. 2011 ‘Fixed partial dentures and crowns supported by very small diameter dental — Major Differences Distinguish Mini Dental Implants from Traditional Dental Implants.’ The Repository, p. 37.
Fraenkel, J. R. & Wallen, N. E. 2001 Educational research: A guide to the process. Mahwah, NJ: Lawrence Erlbaum Associates.
Gratton, C., & Jones, I. 2003 Research methods for sport studies. New York: Routledge.
Helland, A., Wick, P., Koehler, A, Schmid, K. & Som, C. 2007 ‘Reviewing the Environmental and Human Health Knowledge Base of Carbon Nanotubes.’ Environmental Health Perspectives, vol. 115, no. 8, pp. 1125-1127.
Huang, J. S., Zhao, J. J., Liu, Q., & Liu, T. T. 2010 [Clinical research of immediate restoration implant with mini-implants in edentulous space]. Hua Xi.Kou Qiang.Yi.Xue.Za Zhi., 28, (4) 412-416 available from: PM:20848937.
Misch, C.E., Suzuki, J.B., Misch-Dietsh, F.M. & Bidez, M.W. 2005 ‘A Positive Correlation Between Occlusal Trauma and Peri-implant Bone Loss: Literature Support.’ Implant Dentistry, vol. 14, no. 2, pp. 108-116.
Modeland, V. 1998, January ‘Dental Implants; the Latest in False Teeth.’ FDA Consumer, vol. 22, no. 10, pp. 12-13.
Neuman, W. L. 2003. Social research methods: Qualitative and quantitative approaches, 5th ed. New York: Allyn & Bacon.
Pjetursson, B.E., Brägger, U., Lang, N.P. & Zwahlen, M. 2007 ‘Comparison of survival and complication rates of tooth-supported fixed dental prostheses (FDPs) and implant-supported FDPs and single crowns (SCs). Clinical Oral Implants Research, vol. 18, suppl. 3, pp. 97-113.
Price, R. L., Haberstroh, K. M., Webster, T. J. 2004 ‘Improved osteoblast viability in the presence of smaller nanometre dimensioned carbon fibres.’ Nanotechnology, vol. 15, pp. 892-900.
Rushton, M. 2005, September 3 ‘Going to Work Always Puts a Smile on Dr Liam’s Face’: Cosmetic Dental Practice.’ Liverpool Echo, p. 1.
Salinas, T. J. & Eckert, S. E. 2007 ‘In Patients Requiring Single-Tooth Replacement, What Are the Outcomes of Implant- as Compared to Tooth-Supported Restorations?’ The International Journal of Oral & Maxillofacial Implants, vol. 22 (suppl.), pp. 71-95.
Siu, A., Chu, F., Li, T. K., Chow, T-W & Deng, F-L. 2010 ‘Imaging modalities for preoperative assessment in dental implant therapy: an overview.’ Hong Kong Dent J 2010;7:23-30.
Ubell, E. 1992, March 15 ‘They can give you a smile that lasts.’ Parade Magazine, vol. 18, p. 37.
Wood, G. D. & Ellis, R. C. (2003). Risk management practices of leading UK cost consultants. Engineering, Construction and Architectural Management, 10(4), 254-62.

Comments