Traumatic events can shape a person’s life and cause untold stress and pain for long periods of time. Natural disasters occur and can affect a person’s life in terms of losing their home, causing long-term injuries, and creating a sense of instability. Betty has experienced a powerful tornado that ravaged her home and led to her husband breaking his leg. This essay will focus on post traumatic stress disorder (PTSD) assessment and treatment options for someone like Betty to enable her stabilize herself and find ways to positively cope with such trauma.
1.
The first thing to understand is the difference between screening and assessment. Screening involves a typical yes or no answer and evaluation for possible existence of a specific problem. An assessment on the other hand is a process used to define the nature of an issue, determination of diagnosis, and development of specific treatment recommendations to help address diagnosis/issue. Because Betty experienced a traumatic event that result in long-term consequences like losing a home and her husband’s surgery and physical therapy, the first two questions should focus on identifying whether she may display symptoms of PTSD.
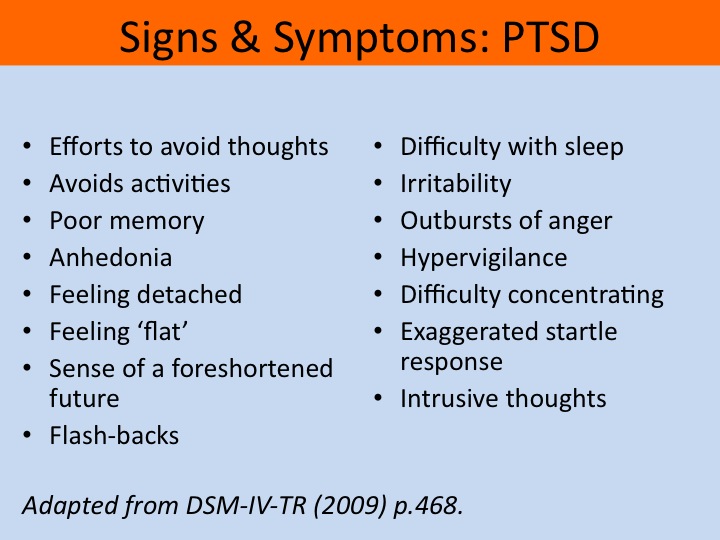
The key reason for PTSD as a possible diagnosis is her re-experiencing of symptoms. Betty stated she relives what happens to her frequently. While she did not say, she has night terrors, or unwanted daytime memories, it seems her reliving the events points to this. Reliving events that are often accompanied by guilt, grief, or other intense emotions can signal PTSD. PTSD is also diagnosed typically following a crisis. “Both Panic Disorder and PTSD are two subtypes within Anxiety Disorders that often are associated with crises” (Cavaiola & Colford, 2011, p. 132).
Therefore, the first question would be: “Do you experience nightmares, flashbacks, or daydreams? If so, what feelings are invoked when you they occur?” This two-part question would be used to confirm what has already been stated by Betty. It will demonstrate she is reliving the trauma in forms that potentially signal PTSD. The answers will also serve as the basis for the PTSD diagnosis.
The next question will center on avoidance symptoms because traumatized individuals try and avoid situations, people, or events that could harken back the trauma experienced. Betty stated her husband needs to have surgery and therapy. She also stated she experiences guilt because she feels she caused her husband’s injury. The question would then be: “What are you trying to avoid, if at all, concerning the night of the tornado?” If she answers her husband, this can help determine the source of her guilt and anxiety and hopefully will be a means of providing treatment recommendations.
The next question would center around arousal symptoms. While Betty has not stated any substance abuse, she may be experiencing some arousal symptoms like feeling easily startled, jumpy, reacting to loud noises, insomnia, and diminished cognitive ability. The 3rd question would then be: “What kinds of behaviors have you exhibited after the tornado?” If Betty needed clarification, some of the arousal symptoms may be provided as examples. This way, she can understand and communicate what has happened to her lately. One important clue of her having arousal symptoms is her inability to sleep due to reliving the traumas.
The fourth question will focus on depression. This is because she has experienced something that has destroyed much of her everyday life. She has nowhere to live, her husband is injured, and she cannot function in the way she could before. The fourth question would then be: “Do you feel hopeless, and if so, why?” People often with PTSD experience depression. Some also experience anxiety disorders and substance abuse. The assessment questions must include a possible diagnosis of depression in order to help Betty deal with any potential hurdles in the future.
The fifth and final question will focus on potential depressive symptoms such as lack of concentration and thoughts of hurting herself. The question would be: “Have you had thoughts of hurting yourself or trouble concentrating on things? What are you having trouble concentrating on? This two-part question will allow the assessment to help navigate what Betty is having trouble with and enable development of a treatment plan/recommendation that will allow her to get back some of the autonomy and independence she had before the tornado. Because Betty was such a prominent figure prior to the tornado, she needs to incorporate some of her former self and former actions into the rebuilding of herself and her life.
2.
The diagnosis code that would be used to diagnose Betty would be (PTSD) DSM-5 309.81 (F43.10). Because Betty experienced symptoms after a traumatic event (the tornado), her symptoms fall under PTSD. While the assessment questions included a potential additional diagnosis of depression, research suggests depression in those that suffer from PTSD may come after the individual experiences a state of ‘emotional numbing’. “Emotional numbing symptom cluster was more strongly related to depression (P < .001) and worse mental health-related functioning (P < .001) than other symptom clusters, while the externalizing behavior symptom cluster was more strongly related to hostility (P < .001)” (Tsai et al., 2015, p. 546). Betty does not appear to display emotional numbing. She feels guilty, she is worried. Therefore, she most likely is not depressed yet.
Now that the diagnosis is PTSD, assessment of her issues and her subsequent needs will be able to allow for a suitable recommendation for treatment for Betty. The two main issues Betty is dealing with are her husband’s surgery and physical therapy and her search for a new home. She feels guilty because her actions (shoving her husband into the basement), led to his leg breaking and then requiring surgery. She needs help in the form of an in-home physical therapy or personal care attendant to facilitate her husband’s recovery.
In relation to finding a new home, because of the tornado, she feels displaced and lacking any foundation from which to recover from her ordeal. Help for her in the form of cognitive behavioral therapy may help her create positive coping mechanisms in order to effectively deal with the stress of her condition and prepare to find a new home and establish herself after the tornado.
3.
The kinds of multidisciplinary referrals needed would be for two things, the first is helping Betty cope with her new life post tornado by establishing healthy coping mechanisms for the stress she must endure to stabilize herself and find a new home. Many that have experienced a traumatic event turn to cognitive behavioral therapy as a treatment option. “Cognitive-behavioral therapy for postdisaster distress (CBT-PD) is a transdiagnostic intervention that has been used following major disasters such as the 9/11 terrorist attacks and Hurricane Katrina” (Hamblen, Norris, Symon, & Bow, 2016, p. 1). The second would be for a social worker so she can be provided options to help deal with her husband’s current state of health. He needs someone there long-term to help him with physical therapy. Betty may have to apply for additional health insurance to cover the costs or see if there is a less expensive alternative to the physical therapy. Physical therapy may cost less if it is done in the home rather than in a medical office.
Research has proven cognitive behavioral therapy (CBT), to be helpful for sufferers of PTSD. “Participants who received intervention early (i.e., 10 to 15 months after Sandy) had the same improvement as those who received it later. Similarly, there was no difference in outcome between individuals with severe as compared with moderate distress at pretreatment” (Hamblen, Norris, Symon, & Bow, 2016, p. 1). Because Betty’s immediate problems are with her husband, and the notion that CBT can be helpful later, it would be most beneficial for Betty to get the CBT referral after she deals with her husband’s problem. His problem requires immediate attention and may help Betty resolve some of the guilty feelings she’s had since the event.
A social worker referral and a referral for cognitive behavioral therapy may help Betty combat the stress that comes from experiencing trauma and help her resolve the long-term problem she has in dealing with her husband’s health condition. She stated she cannot afford long-term physical therapy for her husband. Perhaps with the events that happened, she may qualify for some assistance. She may also be able to apply for health insurance for her husband and discover alternative options for physical therapy that cost less.
It is of high priority that the burden Betty feels concerning her husband is alleviated as it can add to the anxiety and sleep problems she has had from PTSD. One article identifies the risk factors and need for practical assessment strategies to help address the needs of the caregiver and the care recipient.
Risk factors for caregiver burden include female sex, low educational attainment, residence with the care recipient, higher number of hours spent caregiving, depression, social isolation, financial stress, and lack of choice in being a caregiver. Practical assessment strategies for caregiver burden exist to evaluate caregivers, their care recipients, and the care recipient’s overall caregiving needs (Adelman, Tmanova, Delgado, Dion, & Lachs, 2014, p. 1052).
A social worker can help Betty apply for health insurance for her husband that may alleviate the costs of both the surgery and the physical therapy. Additional services should the husband gain better health insurance would be to have a personal care attendant help him in daily tasks.
These two main referrals help resolve the immediate and long-term problems Betty may experience from the tornado-related trauma. She will be able to help her husband through the help of a social worker. She then will be able to help herself with CBT therapy. Each of these referrals not only help Betty, but also her husband in achieving the level of stability they need.
4.
As mentioned earlier, research suggests CBT is an effective treatment option for those with PTSD. The specific kind of CBT that would be useful in the case of Betty is trauma-focused CBT. “Trauma-Focused Cognitive-Behavioral Therapy (TF-CBT) was originally developed for children who had been sexually abused and their non-offending caretakers. TF-CBT was the only intervention that achieved the “well-established” criteria for efficacy” (Mannarino, Cohen, & Deblinger, 2013, p. 165). Since Betty experienced severe trauma due to losing her home and unintentionally injuring her husband as a result of a tornado, she would stand to benefit greatly from this kind of intervention. While TF-CBT was originally used for children, research suggests adults have also experienced positive results from implementation of TF-CBT.
One 2014 study suggested marked improvement in PTSD symptoms following this kind of intervention.
Nine people (5 females and 4 males, mean age 53 years old who had received on average 12 sessions of Trauma-Focused-CBT) who reported a significant reduction in their symptoms following treatment of PTSD took part in semi-structured interviews. Interpretative phenomenological analysis identified five themes: Living with Symptoms before Therapy; Feeling Ready for Therapy; Being Involved; Bringing About Therapeutic Change; and Life After Therapy (Lowe & Murray, 2014, p. 231).
With the evidence suggesting the high rate of efficacy, TF-CBT is the first and main intervention that should be used for Betty’s recovery. It will help her reduce her symptoms she has experienced following the traumatic event. It can help her become aware of any emotions she has not resolved since the traumatic event. Finally, it will give her an opportunity to deal with any painful memories that she experienced while the tornado hit her home.
The next possible intervention is coping skills therapy. While TF-CBT may cover the bulk of problems that Betty may experience due to PTSD, coping skills therapy may help in preventing her from turning to negative behaviors or coping mechanisms to deal with the stress and problems she currently faces. One study examining the effective of coping skills therapy on PTSD showed marked improvement in sufferers in terms of symptoms and interpersonal problems. “We found medium to large effect sizes for improvements in PTSD symptoms, general psychopathology, and interpersonal problems at end-of-treatment, all of which were sustained at follow-up” (Kaiser et al., 2015, p. 401).
Developing positive coping skills is important in any case of psychological trauma. If Betty does not learn how to properly deal with the various symptoms she is experiencing, she could spiral down and become depressed. She may also not be able to handle the responsibilities she has, prompting her condition to worsen. She must deal with her problems in a positive and effective way if she is to successfully handle the trauma of the tornado.
The third and final intervention that can help someone like Betty get past her experienced trauma is a pharmacological-based intervention. Betty states she has trouble sleeping because she relives the events of the trauma. Zaleplon while not used as treatment for PTSD, may serve to help that need sleep but do not want decreased responsiveness. “…because of its short length of action, zaleplon may be a good choice for those traumatized individuals who are particularly concerned about sedation and decreased responsiveness to threats” (Briere & Scott, 2014, p. 319). It is a short-term solution to help Betty get some rest so she can make sound decisions for her future.
The three interventions listed are treatment options that deal with both the short-term and long-term effects of PTSD. These interventions are TF-CBT, coping skills therapy, and a prescription of Zaleplon for sleep. Betty will be able to reduce her PTSD-related symptoms with such treatment options. She will also be able to get immediate relief in terms of sleeping. This will hopefully lead to her developing positive coping skills and have the fortitude to continue on and build a solid foundation after experiencing the events of the tornado.
In conclusion, Betty may have PTSD. To help Betty deal with the symptoms of PTSD, she needs TF-CBT as a main intervention, along with coping skills therapy, and a prescription of Zaleplon. Referrals for Betty must be aimed towards helping her address her to main concerns. Those concerns are symptoms of PTSD and her husband’s health. A referral to a social worker can help Betty gain information and possible strategies to help her deal with her husband’s surgery and subsequent need for physical therapy. A CBT referral can help her cope with the symptoms of PTSD.
Adelman, R. D., Tmanova, L. L., Delgado, D., Dion, S., & Lachs, M. S. (2014). Caregiver Burden. JAMA, 311(10), 1052. doi:10.1001/jama.2014.304
Briere, J., & Scott, C. (2014). Principles of trauma therapy: A guide to symptoms, evaluation, and treatment.
Cavaiola, A. A., & Colford, J. E. (2011). Crisis intervention case book. Belmont, CA: Brooks/Cole Cengage Learning.
Hamblen, J. L., Norris, F. H., Symon, K. A., & Bow, T. E. (2016). Cognitive Behavioral Therapy for Postdisaster Distress: A Promising Transdiagnostic Approach to Treating Disaster Survivors. Psychological Trauma: Theory, Research, Practice, and Policy. doi:10.1037/tra0000221
Kaiser, D., Grundmann, J., Schulze, C., Stubenvoll, M., Kosar, M., Junker, M., … Schäfer, I. (2015). A Pilot Study of Seeking Safety in a Sample of German Women Outpatients with Substance Dependence and Posttraumatic Stress Disorder. Journal of Psychoactive Drugs, 47(5), 401-408. doi:10.1080/02791072.2015.1090644
Lowe, C., & Murray, C. (2014). Adult Service-Users’ Experiences of Trauma-Focused Cognitive Behavioural Therapy. Journal of Contemporary Psychotherapy, 44(4), 223–231.
Mannarino, A. P., Cohen, J. A., & Deblinger, E. (2013, October 9). Trauma-Focused Cognitive-Behavioral Therapy – Springer. Retrieved from http://link.springer.com/chapter/10.1007/978-94-007-7404-9_10
Tsai, J., Harpaz-Rotem, I., Armour, C., Southwick, S. M., Krystal, J. H., & Pietrzak, R. H. (2015). Dimensional structure of DSM-5 posttraumatic stress disorder symptoms: results from the National Health and Resilience in Veterans Study. The Journal of Clinical Psychiatry, 76(5), 546-553. doi:10.4088/jcp.14m09091
